What is it like to have CAD?
Symptoms of CAD include chest pain, palpitations, abnormal heart rhythms, shortness of breath, and swelling in the extremities. Of course, these are also symptoms of HCM and many other heart diseases. Unfortunately, many people do not experience symptoms in the early stages of this disease. The disease progresses until the blockage causes symptoms. If the blockage becomes severe enough, a heart attack (myocardial infarction) is the result. This can lead to death of some of the heart tissue, and further problems. CAD is usually diagnosed with stress tests and cardiac catheterization.
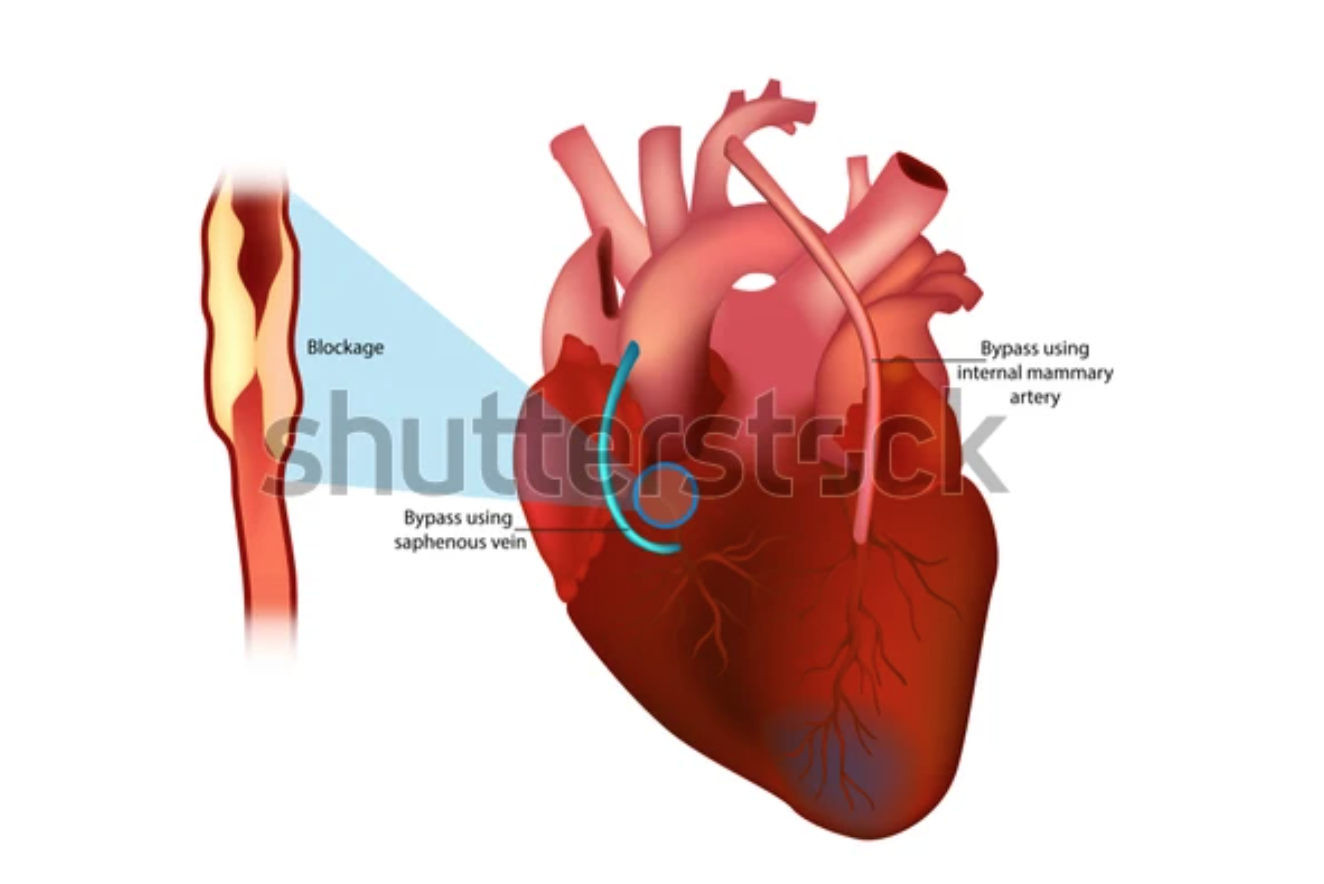
Bypass surgery
One way to treat a narrowed or blocked artery is to bypass it with a piece of a healthy blood vessel (graft). The graft can be a piece of a vein from your leg or artery from your chest or wrist. It is lucky that we have somewhat more blood vessels than we really need - your circulation will be fine even without that vessel that the surgeon repurposed! One end of the graft is attached above the blockage and the other will be attached below to bypass the blocked section.
Sometimes people have multiple arteries that are blocked. These can be bypassed as well. That is what is meant when you hear that someone had a triple bypass or a double bypass.
Risks
CABG is major surgery, so it has risks. But it is the most common open-heart surgery, so a lot is known about how to perform it and how to minimize risks. The risks include bleeding during or after surgery, blood clots, incision site infection, pneumonia, pancreatitis, kidney failure, graft failure, and death. The surgeon will discuss with you any additional risks due to your particular condition.
Preparing for the Surgery
Bypass surgery is like any other surgery in many ways. You will have a number of diagnostic tests before the procedure. The surgical team will discuss with you what drugs you should or shouldn't take beforehand, and when you need to stop eating and drinking. They will ask about bleeding issues and may have special instructions if you are taking drugs that hinder clotting of blood (anticoagulant drugs). If your surgery is planned, and not an emergency, stop smoking beforehand. Of course you should not start again afterward!
Recovering in the Hospital
You will be taken to the intensive care unit (ICU) to be closely monitored. CABG surgery requires staying at the hospital for at least several days after the procedure. You will most likely have a tube in your throat so that a ventilator can help you breathe until you are stable enough to do it on your own. As you wake up from the anesthesia and begin to breathe on your own, the setting on the ventilator can be adjusted so that you can do more of the breathing by yourself. When you are awake enough to breathe completely on your own and can cough, the breathing tube will be removed. In most situations, the breathing tube is removed on the same day as the surgery or by early the next morning. Your stomach tube will also be removed at this time. Once the tubes are removed and you are stable, you can start to drink liquids. You can slowly incorporate solid foods when you can handle them.
It is important that you cough and take deep breaths every couple of hours after your breathing tube is removed to help prevent mucus from collecting in your lungs and causing pneumonia. It will be uncomfortable, but your nurse will show you how to hug a pillow tightly against your chest to help the discomfort.
The incision site may continue to be sore for several days after the procedure. You will be given pain relievers as needed, as well as other drugs to stabilize your blood pressure or control bleeding.
When you are ready, you will be moved from the ICU to a post-surgical unit where you will continue to recover. You can gradually increase your activity and get out of bed and walk for periods of time.
Recovery at Home
Once you are discharged and home, pay close care to make sure the incision area is clean and dry. Your doctor will give you specific instructions on how to bathe. If your sutures or staples were not removed before leaving the hospital, they will be removed during a follow-up visit.
Do not drive until your doctor allows you to do so. Your doctor may also place other activity restrictions on you, including limits on the amount of weight you can lift.
Be sure to tell your doctor if you have any of the following:
-
- Fever of 100.4° F (38° C) or higher
-
- Redness, swelling, or drainage from the incision sites
-
- Increased pain around the incision sites
-
- Swelling or numbness in the extremities
-
- Persistent nausea or vomiting
Your doctors will recommend an exercise program (emphasizing walking) for you to help you recover. Follow it! Do not push yourself to do things that are not comfortable, but in general the more you walk, the faster you will recover. They may also recommend that you take a cardiac rehabilitation class after some weeks. If you are able to do so, it is a great idea.