originally posted February 24, 2017 Huffington Post by Lisa Salberg
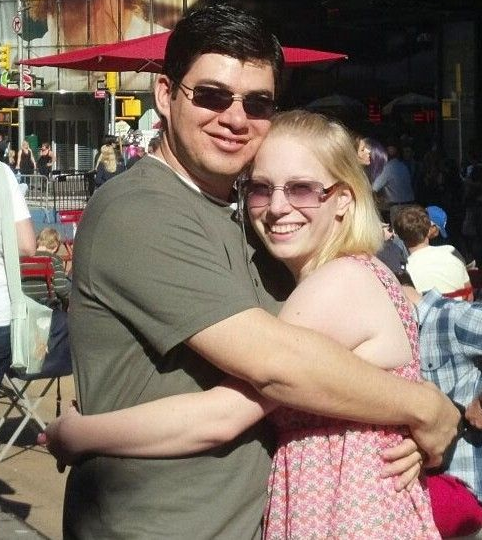
So there I was holding my heart in my hands while a new heartbeat was in my chest. Talk about surreal moments! The path that led to this moment encompasses 36 of my 48 years on this earth and in this one moment, I came face to face with the very thing that I had hated, feared, and loved… my heart.
The story actually begins far before my birth and continues past me to my daughter, niece, and nephew. These are stories for another day. Today I want to tell you about the first and last chapter of my heart. In the next installment, I will tell you what is in store for her future, because yes, she has an important future.
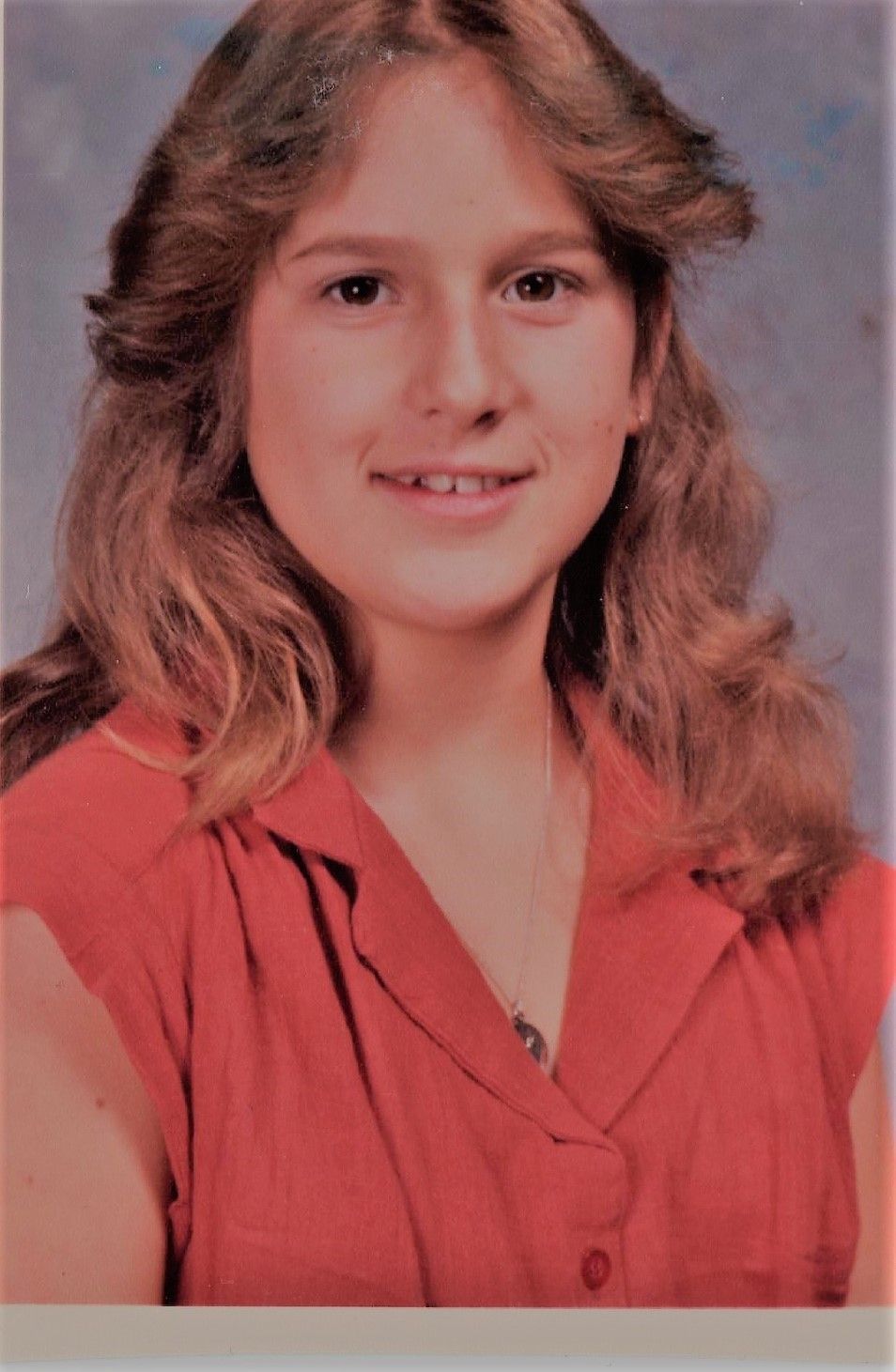
I was diagnosed with hypertrophic cardiomyopathy when I was 12 years old. I was in the 7th grade at Copeland Middle School in Rockaway NJ and it was physical day. You remember those awkward events when all the girls had to take their shirts off down to bras and have the doctor listen to their heart and the nurse check for scoliosis. When I stood before the doctor, his face dropped and he told the nurse to clear the room. He then had the nurse listen as well. I knew right then that the same disease that had killed my grandfather at 43, impacted my uncle and sister, had just shown its ugly head, and my life was forever changed. I was told I had to see a cardiologist soon or not be permitted back in school. After the consult with Dr. Paul Goldfinger, he confirmed the diagnosis (then called Idiopathic Hypertrophic Subaortic Stenosis IHSS – now called hypertrophic cardiomyopathy-HCM). My first question was “do I have to do my homework?” Why that question? Because he had just told me, in 1980, there was no real treatment, no cure, and I could die suddenly at any time. Did I mention I was 12?
In my next posts, I will fill in the years between and explain far more about HCM, healthcare policy, and how it has impacted my life and the lives of those I serve as CEO/Founder of the Hypertrophic Cardiomyopathy Association. But now let’s flash forward to September 2016.
HCM is a highly variable disease, some people have minimal to no symptoms at all while others are severely impacted. I spent much of my life living on a balance beam to manage symptoms. In 2011, I found out that my heart was becoming too stiff and the ejection fraction (the amount of blood your heart process per beat) had dropped. This was the indication that transplant would be my only option but I had to get sicker before I could list. You must understand that heart transplantation is NOT given to improve symptoms it is ONLY given to save a life. So you have to be well enough to withstand the surgery and sick enough to be “terminal” without the transplant.
September 2016 was a busy month for me work-wise and an exciting one. I was invited to a meeting at the White House to discuss “Cardiovascular Health in America”. This was my second time participating in this event. While I stood there to make a statement about the importance of better understanding genetic causes of heart disease something happened I felt my heart acting strange and I had to stop speaking and ask for a moment. Little did those in the audience know, I nearly passed out. I regained myself and acted as if everything was fine – I am good at that. I returned home and the next morning attended a wedding, then home for a nap because my daughter had gotten us tickets to a concert. Ironically, it was Joan Jett and the Blackhearts and Heart (a double heart concert). Sunday I rested. Monday I flew to Grand Rapids Michigan to review a new HCM program at Spectrum Health. I spent two days there and flew home Wednesday to a meeting at Morristown Medical Centers Chanin T. Mast HCM program. This is where I also received my own care for HCM under Dr. Martin Maron. When I got to the meeting, my nurse Deatrah Debose said I didn’t look right. I told her I didn’t feel right but I’d rest for a day and if I was not better I would come in for some IV Lasix therapy to get the extra fluid off of me. Friday I admitted myself. Saturday the Lasix took off 6 pounds, but I didn’t get better, I got worse. I laid in bed with oxygen and knew this time I was really in trouble and I knew where this was leading. I shut down I could hardly speak. My mind raced to my family, my community, my work how was I going to do all I wanted to do. Wait, none of that mattered anymore. How was I going to survive, that is all that mattered.
Monday a right heart catheterization indicated that my heart was simply not working anymore. My “cardiac index” which should be 2.2-4.1 was only 1.4. My heart was simply not moving blood anymore. I was given a PICC line with a medication called milrinone which did improve my index to 1.8 and I was sent home to begin the listing process. It took 2 months to complete the tests and classes and review to be listed. On November 23 I was officially listed on UNOS as a status 1B for transplant. I will explain more about this process in the future.
I did, however, make a deal with my transplant center Newark Beth Israel Medical Center. I must KEEP my heart . I wished to use it as a teaching tool. I did not think this was so strange, but as it turns out I was the first person to make this request at this hospital. I made arrangements with a program that specializes in Plastination, a process that makes organs last forever. I arranged the logistics in advance and asked my husband to please ship my heart away after my transplant (it didn’t sound odd at the time, but after it was done I wondered if I had really considered how this impacted him … he survived so I guess it wasn’t that bad).
Groundhogs day 2017 12:23 am the phone rang. “ Lisa? This is Emily from Newark Beth, we have your heart. How soon can you be here?”

The post Lisa, we have your heart. How soon can you be here? appeared first on Hypertrophic Cardiomyopathy Association.
HCMA Blog

 Translate
Translate