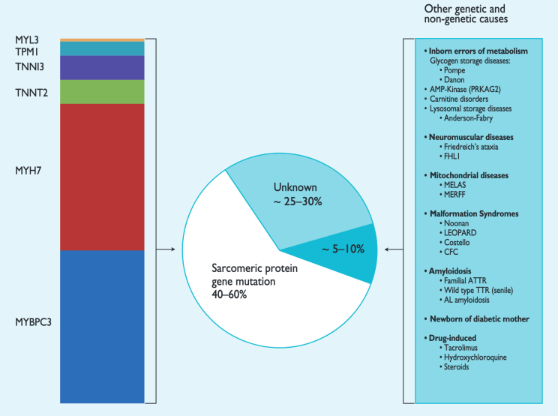
Not all big hearts are the same. Cardiomyopathy may result from various genetic or environmental factors. Not ALL thick hearts are Hypertrophic Cardiomyopathy, some have been called "mimickers" or phenocopies. It is important to know WHY your heart is thick and genetic testing, review of symptoms and family history may lead you to treatment options that are targeted at the reason YOUR heart is thick.
HCM phenocopies
• Can look just like HCM
• Are important to identify
• Have a different disease course
• Have systemic manifestations
• May have potential targeted treatment
Elliott PM et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and
Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014 Oct 14;35(39):2733-79.
Why do hearts become thick?
Amyloidosis
Read MoreAmyloidosis is rare, and there are several types. Two types can cause a thick heart like HCM. ATTR amyloidosis looks the most like HCM. Some "HCM patients" may actually have amyloidosis.
Danon Disease
Read MoreDanon Disease is very rare. Up to 4% of "HCM patients" actually have Danon Disease. Most people with Danon have heart problems.
RASopathies
Read MoreRASopathies are rare and include several different conditions. The most common is Noonan Syndrome. These syndromes are typically found in childhood, but later diagnosis is possible. Most RASopathy patients (up to 80%) have heart problems, including congenital heart defects and "HCM".
Fabry Disease
Read MoreFabry Disease is rare. There are classic and late-onset forms. About half of Fabry Disease patients have heart involvement. Late-onset Fabry includes "HCM appearance" in half of male patients and a third of female patients.
Pompe Disease
Read MorePompe Disease is very rare. It is usually diagnosed in infancy, but it can be diagnosed later. Almost all cases of Infantile Pompe involve the heart, with 92% having the appearance of HCM. About 12 of every 100 adult Pompe patients have a heart problem, usually "HCM".
Friedreich's Ataxia
Read MoreFriedreich's Ataxia (FA) is very rare. More than half of adults with FA have heart problems, often "HCM". FA also causes muscle weakness and other issues.
PRKAG2
Read MorePRKAG2 Syndrome is very rare. About 1 of 100 "HCM" cases is caused by PRKAG2 Syndrome. Up to 70% of those with PRKAG2 have heart disease. It affects other body parts, such as the brain, liver, kidneys, pancreas, and muscles. The name is based on the gene that causes this syndrome.

 Translate
Translate