The HCMA: A home for the Bighearted
Not all big hearts are the same
The Hypertrophic Cardiomyopathy Association (HCMA) is here to help you understand more about your big heart.
The HCMA offers Support, Education, and Advocacy for Hypertrophic Cardiomyopathy (HCM) - Empowering patients and advancing research for a brighter future.
Should you have questions at any point while reviewing this website, please reach out the the HCMA office at: 973-983-7429 or email us at support@4hcm.org and we will respond as soon as possible.
The HCMA
offers the following
services, educational resources, and support
to empower you no matter where you are in your HCM journey.
Some big hearts are thick and stiff because of Hypertrophic Cardiomyopathy
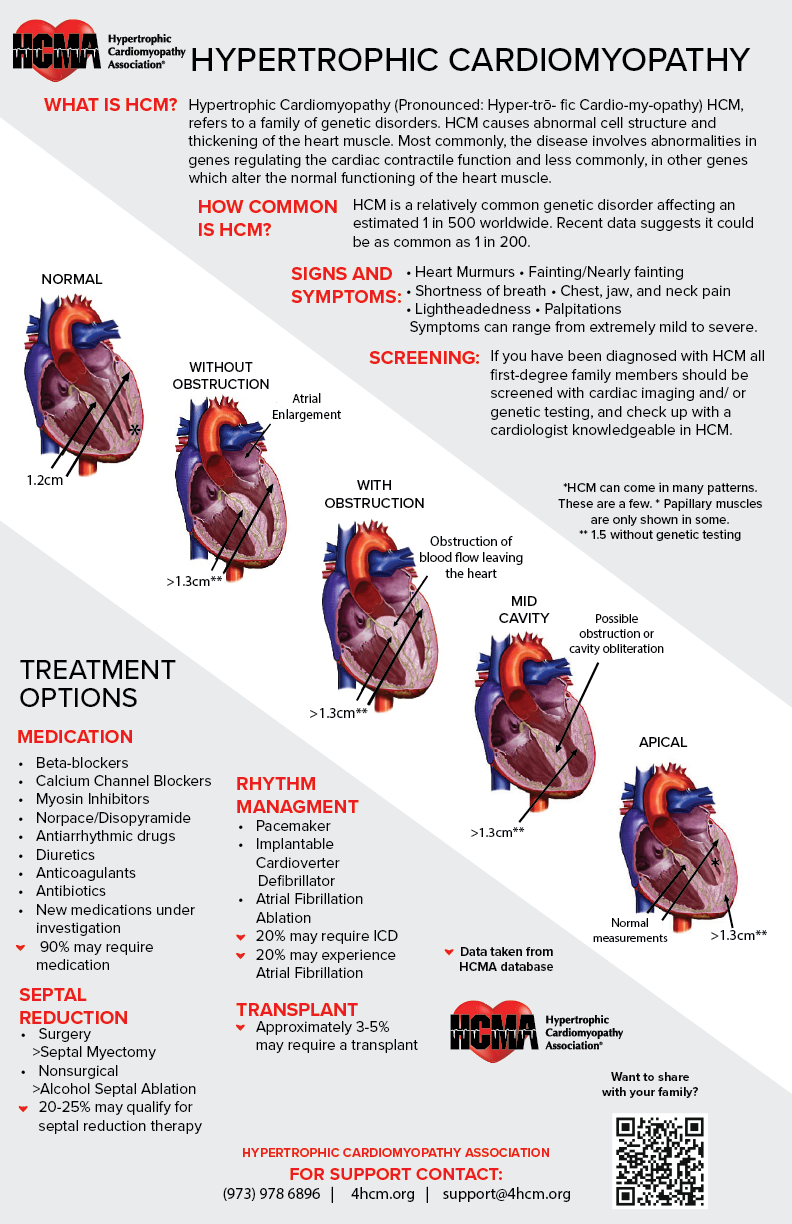
Hypertrophic cardiomyopathy (HCM) is a common genetic disorder that affects people regardless of gender, ethnicity, age or geographic location.HCM is known by many names and it is important to understand that it is, for the most part, one disease.
More about HCM
Oftentimes, those with hypertrophic obstructive cardiomyopathy(HOCM, oHCM), apical hypertrophic cardiomyopathy, or asymmetric septal hypertrophic cardiomyopathy think this is a completely different disease, when in reality, it is all hypertrophic cardiomyopathy with varied physical presentations. To phrase it differently, the words "obstructive," "apical," or "asymmetric septal" are just descriptions of the current state of the disease.
This website will expand your knowledge of hypertrophic cardiomyopathy as well as issues important to our community by providing clinically reviewed information, support options and member services.
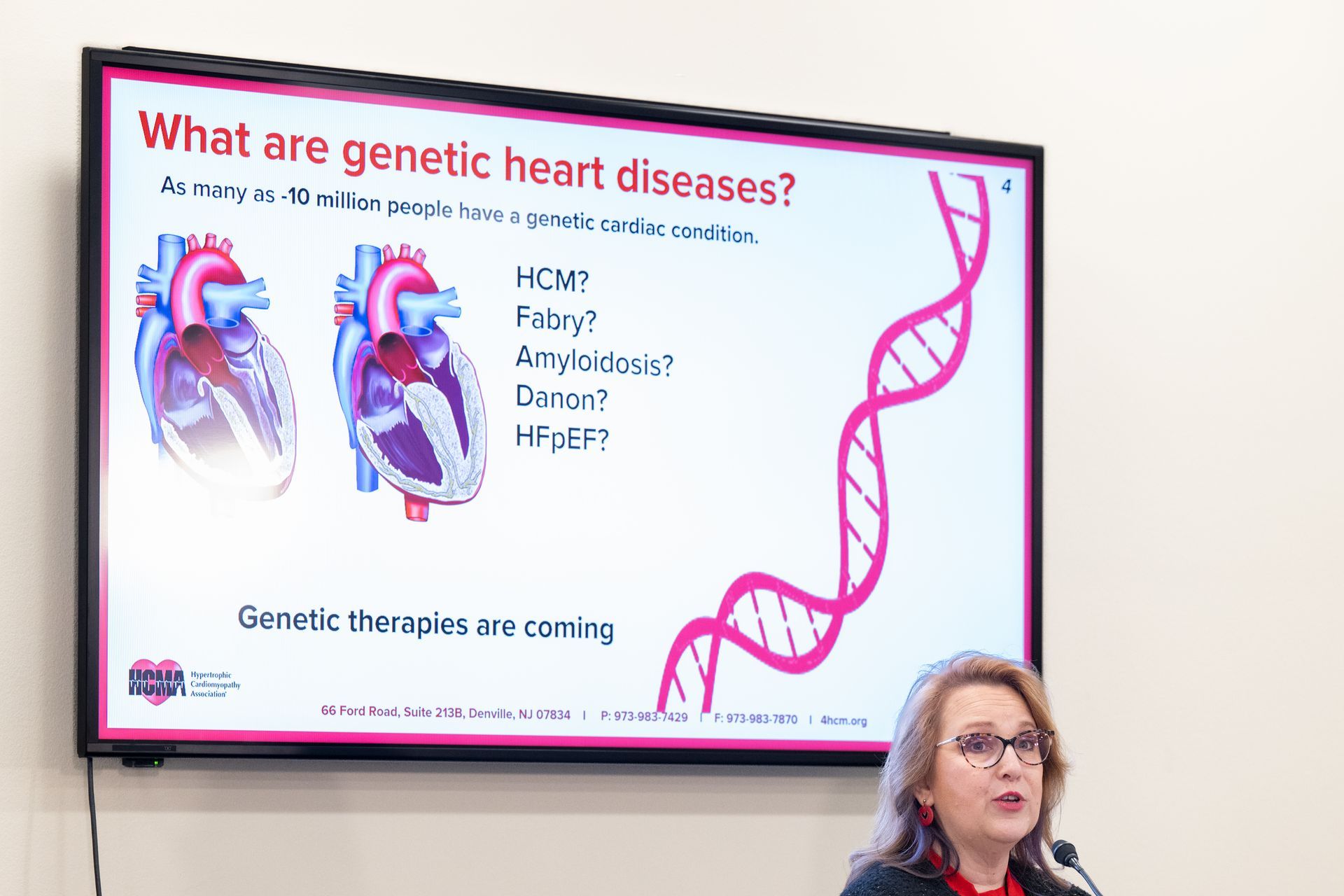
Watch the 2025 HCM Awareness Day Webinar
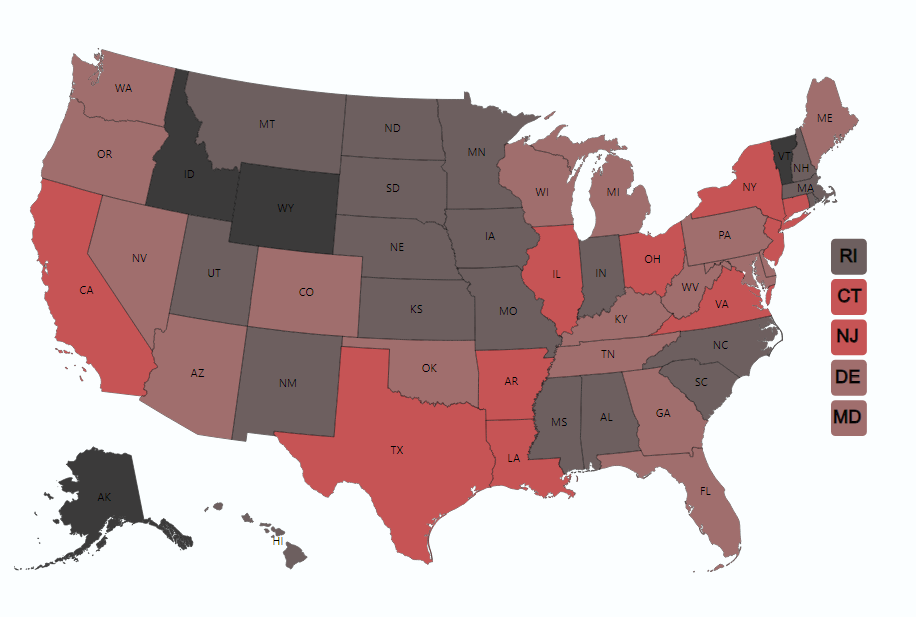
The Children's Cardiac Safety Act Report Card
How is your state doing regarding helping to find the undiagnosed?
Click on the map to learn more about initiatives in your state and how you can help!
If you find an error in your state data please send us a report!
Submit a Report Card Correction
It only takes three clicks to save a life. Act now to support the
Children's Cardiac Safety Act legislation in your state.

 Translate
Translate